This is part of a series of blog posts around Pacing which is mainly aimed at people who have ME but may also be relevant for other Spoonies such as those with Fibromyalgia or PoTS.
NB I’ve re-edited the post because I wasn’t completely happy with the clarity and format before. Hopefully it is now a bit clearer and easier to read. Some of the content has been taken out to go into a separate quick tips for Pacing post.
At some point I’ll try to record this onto Soundcloud, let me know if you’d benefit from this (to give me some motivation!).
See sidebar warning>
Pacing
Personally I’m revisiting the basics of Pacing, because now the beta blockers are easing my immediate Post Exertional Malaise from POTS I’m having to plan for the delayed PEM from ME. Believe it or not this is what they call a better class of problem!
The CFS/ME working group report on CFS (2002) describes Pacing as follows:
“Pacing is based on the envelope or glass ceiling theory of CFS/ME which suggests that energy is finite and limited, and that the best way for a sufferer to manage their illness is to live within this envelope i.e. not constantly break through the ceiling (some advise never going beyond 70% of a sufferer’s perceived energy limit)”.
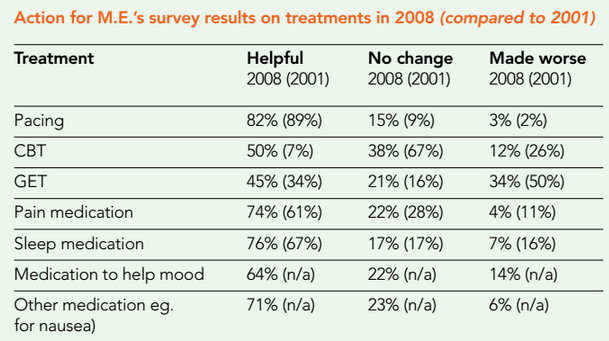
Accepting Sceptics’ view^: Surprisingly the controversial PACE Trial didn’t show Pacing to be effective. However, this result lacks face validity (i.e. even glancing at the results it looks like they may not be measuring what they think they’re measuring) as patients consistently report Pacing as a helpful approach:
(copied from here) and other research tends to indicate positive results from different forms of Pacing (see Goudsmit et al 2012). There is even suggestion that Adaptive Pacing isn’t Pacing (ie they weren’t measuring Pacing afterall), which illustrates how confusing this is to navigate as a patient with brainfog!
Pacing, CBT, GET, It Gets Confusing
If you’re newly diagnosed (or just revisiting techniques during a bad relapse) it can get quite overwhelming to disentangle what people mean by these different terms for ME activity management, especially as so much health politics seems to be in the way.
These 3 approaches to treatment come from different theoretical perspectives on the nature of why you have to manage activity levels. Pacing comes from the perspective that you are physiologically ill and limiting activity allows the body to have energy to heal itself (similar to resting when you have flu). The other two approaches have quite a different understanding of the nature of CFS which they see as due to deconditioning and/or false illness beliefs (so practitioners using GET or CBT techniques will be less concerned about the danger of relapse and more interested in the importance of increasing activity). Depending on what your personal views are about the nature of your illness, you’ll want to keep your eyes open to this through the brainfog.
This table from the PACE study will help you identify which perspective someone is coming from (APT is the form of Pacing they used as a comparison to Graded Exercise and a CFS version of CBT):
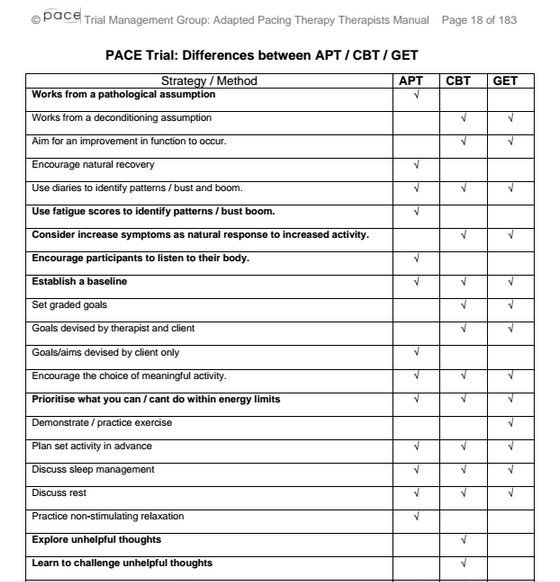
P18 (this table is worded to be acceptable to all 3 practitioners and is in their own discourse but other people would query the relevance of “unhelpful thoughts” etc).
There seems to be general agreement between patients that Pacing is a “good thing” and Graded Exercise can be dangerous. However, there also seems to be quite a bit of variation in what people actually do in practice under the label of Pacing.
Methods of Pacing I’ve come across over the years include a mathematical approach (carefully measuring activities by timing or distance); Symptomatic (stopping based on increased symptoms); Bouncing the Boundaries (more of an art than a science); alternating activities (you may be too tired to continue one activity but changing activities can be OK); Adaptive Pacing (a more structured and planned approach) and heart rate monitoring.
Some of these approaches are usually combined with other aspects of an ethos. For example, heart rate monitoring can include a pacing style such as staying under a personal beat per minute but also a tactic more similar to Graded Exercise of planned increase in exercise (while staying under the ceiling heart rate). Bouncing the Boundaries is likely to be combined with relaxation activities and a change of diet. The rest of this post will cover a few of my personal observations about different style of Pacing.
Pacing by Numbers
The simplist model of Pacing to describe, but perhaps the hardest to live by, is the mathematical one. This is considered a bit out of date but is useful to illustrate the idea of pacing and may help you. I have never managed to do this properly so I can’t write an authentic review.
What to expect:
1. Your activity level is making you worse (eg walking for 9mins)
2. Reduce to a level you can sustain for 3 days in a row (eg 6mins)
3. Halve this = your new baseline activity level (eg 3min walking)
You would do this for different activities such as watching TV, so if you can sustain watching 2 episodes of The Good Wife on the same day, only watch one. TV viewing gets complicated though because as discussed previously (link) some programmes are less demanding.
Accepting Sceptic: When you try to live this model out you realise that everything is complicated and some practical tasks are pointless if split in half. Who has a reason to walk exactly 3 minutes a day? When we’re at that level we don’t really want to walk 3 minutes for no reason and then have no energy to do something useful like wash.
Also, once you’ve halved all your activities, what do you do with the rest of your (now abundant) spare time? It isn’t realistic to spend all day meditating. Inevitably you’ll spend too long doing something, such as worrying or obsessing over the timing of activities…
Helps with: I do think this is a useful illustration of the idea of Pacing though. For example, it’s not just about what you can sustain but keeping some energy back for your body to use in healing. The Spoon Theory is similar (link).
It can also be useful if applied to one particular activity in isolation. For example, I haven’t been well enough to cook for myself. To get back into this activity I could carefully time different cooking activities in terms of how long standing. When I’ve built up to a time that makes me a little worse I then reduce again to a sustainable amount and then do half that. This would be better than just not doing the activity (but I would probably only eat toast).
Side effects/cautions: Always be cautious about adjusting activity levels with ME (and other spoonie conditions).
What do I do?
Although I’m not a good advert for any approach at the moment, as I’m virtually housebound, I have previously got to around 90-95% recovered. I’ve been trying to think about which styles of pacing have worked for me before. [I don’t know how much of my problem is PoTS rather than ME though, and that can go into spontaneous remission. Personally, I think which type of pacing you respond to may be a lot to do with the CFS/SEID subgroup you belong to and there isn’t enough information about this yet].
Tickling the Boundaries
I’ve mostly used an intuitive, unstructured approach (partly because I wasn’t taught anything structured in the early years). This is similar to the Optimum Health Clinic’s Bouncing the Boundaries. I don’t have a precise, measured baseline but if I think about it I do have a baseline because I have a fairly accurate idea of what I can sustain on a daily basis and at what point I’ll need to be cautious. I have a general sense of what I can maintain activity wise (vaguely separated in my mind into physical, mental, social) and I try to keep to this for a phase of time. If I know I have to spend more energy than this informal baseline I ‘rest up’ before and after in proportion (this could be a week or an hour depending on how big the event is). I try to balance different types of activity.
When I get consistently bored rather than over-tired or more ill I try to do a bit more. If I’m OK with this in terms of no increase in symptoms, fatigue or noticeable PEM, it is part of my new routine, if not I step back again. Building up walking in this way helped me but I mainly walked purposefully, such as to go shopping, rather than for the sake of exercise. When I built up working I took on separate bits of voluntary and part-time work, so that I could add and drop activities without having to give up everything if I got worse for a while. I got to the equivalent of full-time work doing this but unfortunately, after a kidney infection, I had to gradually reduce workload again.
Heart-rate Monitoring
I find a heart-rate monitoring method of pacing/activity management useful (see this post which explains it in more detail), and I suspect this is useful for other people in the PoTS-ME subgroup. Initially I learnt what my morning resting rate should be and a raise in this was a warning to cut back. I found out which activities put my heart rate over 110bpm and avoid them (initially every time I stood but now on beta blockers its things like making the bed or walking upstairs too quickly). This does appear to relate to Post Exertional Malaise. I am now doing gentle, lying down yoga a couple of times a week because my heart rate stays low and I don’t seem to get a PEM backlash. I don’t seem to need to stick to the exercise plan for this because my heart rate stays so low.
Question:
Do you know anyone with PoTS and ME who has successfully increased activity without using GET? I’d like some tips on the next stage that is sympathetic to both conditions. I’ve heard that potsies do well with non-standing exercises like rowing machines, recumbent bikes and swimming but that will be too much exertion for my ME at the moment. I’m not well enough to go to classes so YouTube links much appreciated.
Conclusion
When it comes to activity management in ME, this fake Buddha quote often pops into my mind:
“Believe nothing, no matter where you read it, or who said it, no matter if I have said it, unless it agrees with your own reason and your own common sense.”
A follow up post with quick tips on Pacing is in process (click here).
Further reading:
Action for ME booklet
Bouncing the Boundaries
Goudsmit et Al (2012) for a more academic overview
Adaptive Pacing Manual (see resources at the end)
Key:
- Accepting Sceptic comments on this site can be alternative explanations or queries based on critical thinking. They are often comments which are accepting that an approach is of benefit to Spoonies but sceptical because it may be for reasons other than the official sales patter.
great blog. thank you!
LikeLiked by 1 person
Pity you didn’t read the review in Disab Rehab, which provides a definition, scientific rationale, and reasons why APT is NOT, pacing. The above is lay stuff based on misunderstanding and old work on chronic pain. There is scientific evidence supporting pacing for ME. You haven’t described any of that though. Surely you must have been aware of it? Action for ME are not reliable s far as pacing is concerned and if you had read the scientific blurb, you’d see the major differences between pacing and GET (they are opposites). I don’t understand APT on any level. I don’t have a baseline. Everyday is a new experience.
LikeLike
Hi Ellen. This is a lay opinion based on my experience. Could you be more specific on what I’m misunderstanding (or misexplaining)? Perhaps I’m missing out on getting better quicker by not getting this straight in my head. I do find Pacing helpful but I’ve sort of evolved my own form of it. I’ve actually not seen much research on Pacing (is it maybe the bio research that is always being shared?)
LikeLike
Ellen, I’ve found your paper from 2012. Is this what you’re referring to from Disability Rehabilitation? I’ll give it a read.
LikeLike
I’ve added a reference and can see there are some extra tips to add to the post when my Pacing allows… I’m not getting how ApT isn’t Pacing though, perhaps I will tomorrow.
LikeLike
Pingback: Resource: Quick Tips for Pacing | Tips for ME
Pingback: Is it About Getting Better or NOT Getting Worse? | Tips for ME